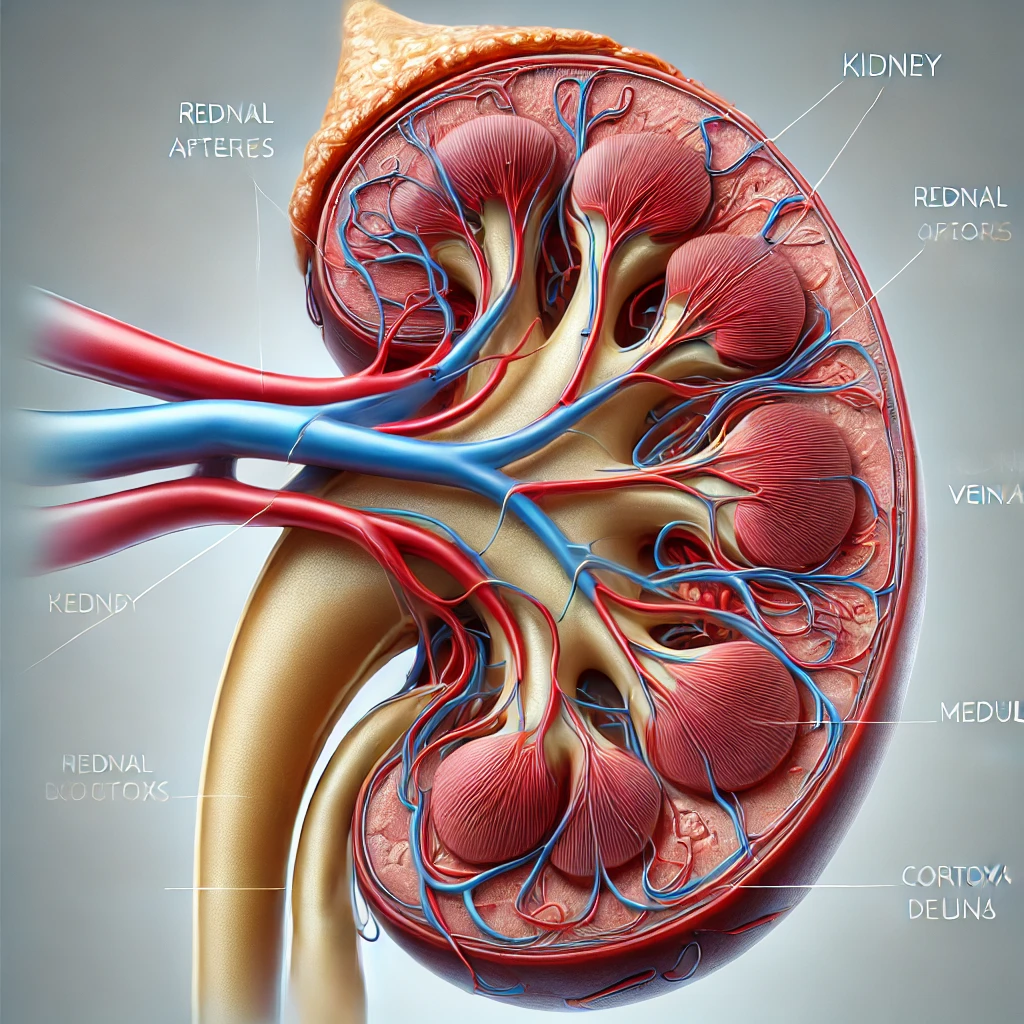
Kidney disease alcohol consumption, Can Drink Alcohol?
1. Can People with Kidney Disease Drink Alcohol? Kidney disease alcohol consumption, Chronic kidney disease (CKD) impairs the kidneys’ ability to filter waste effectively. This raises an important question: Is alcohol consumption safe for CKD… Kidney disease alcohol consumption, Can Drink Alcohol?