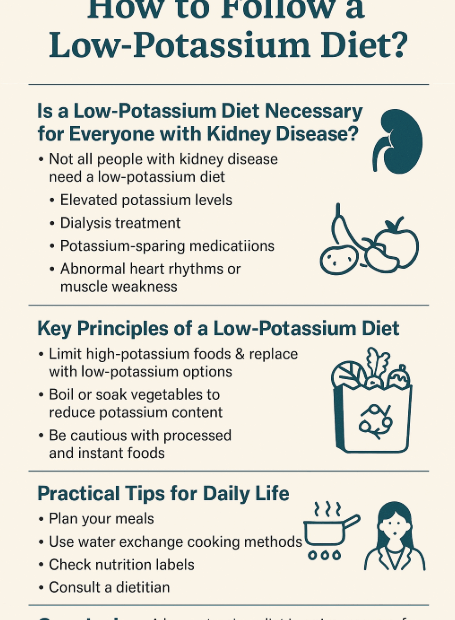
How to Follow a Low-Potassium Diet?
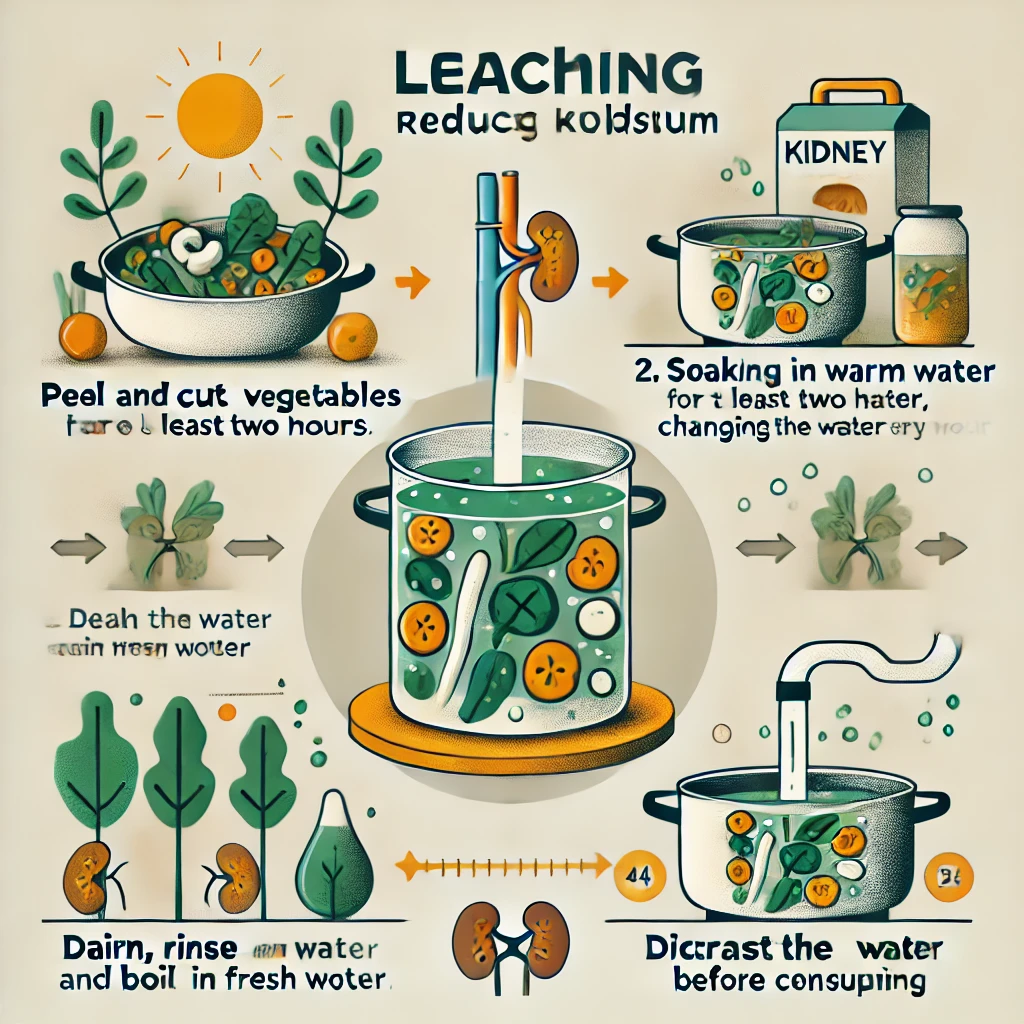
Potassium is an essential mineral that helps regulate heart function and muscle contractions. However, for people with chronic kidney disease (CKD), those undergoing dialysis, or those with certain health conditions, managing blood potassium levels is… How to Follow a Low-Potassium Diet?