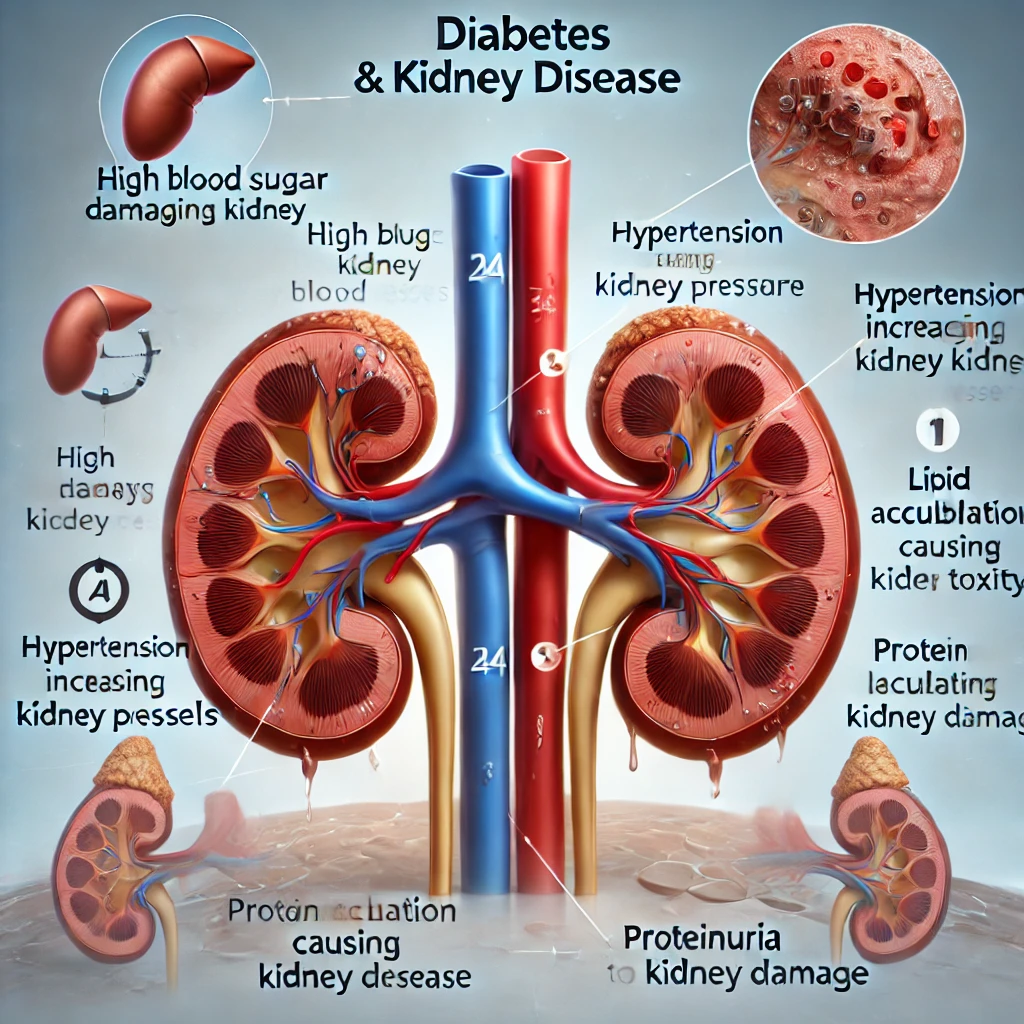
Diabetes and Kidney Disease: Why Do They Occur Together and How to Manage Them Effectively?
🔸 Summary of Key Goals Blood Sugar Control: HbA1c 6.5–7.0%, Fasting Blood Glucose 80–130 mg/dL Blood Pressure Control: Below 130/80 mmHg Proteinuria Reduction: UACR <30 mg/g, at least 50% reduction if present Dyslipidemia Management: LDL… Diabetes and Kidney Disease: Why Do They Occur Together and How to Manage Them Effectively?