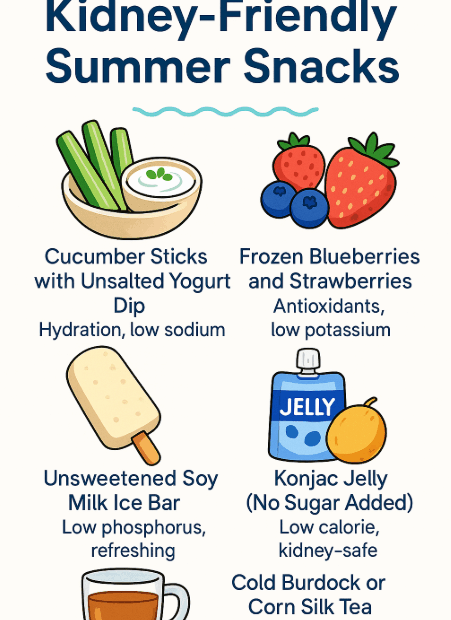
Kidney-Friendly Summer Snacks: Refreshing & Safe Choices for Your Health
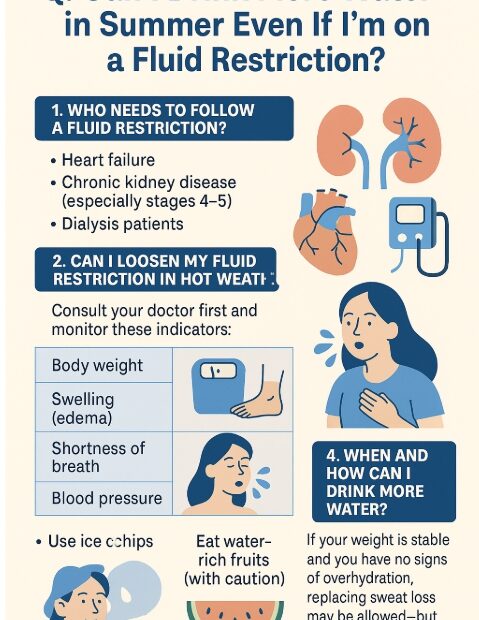
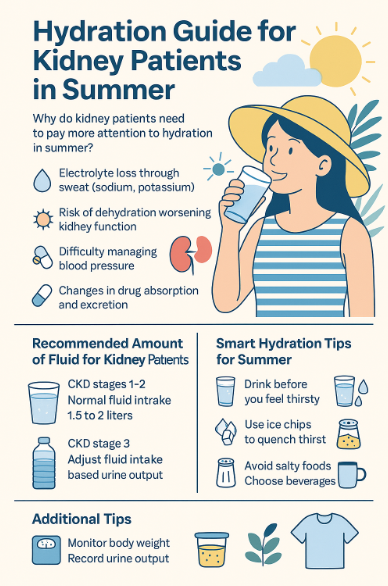
Summer can be challenging for people with kidney disease or anyone wanting to protect their kidney health. High temperatures increase the need for hydration, but many common summer treats are full of sugar, salt, or… Kidney-Friendly Summer Snacks: Refreshing & Safe Choices for Your Health