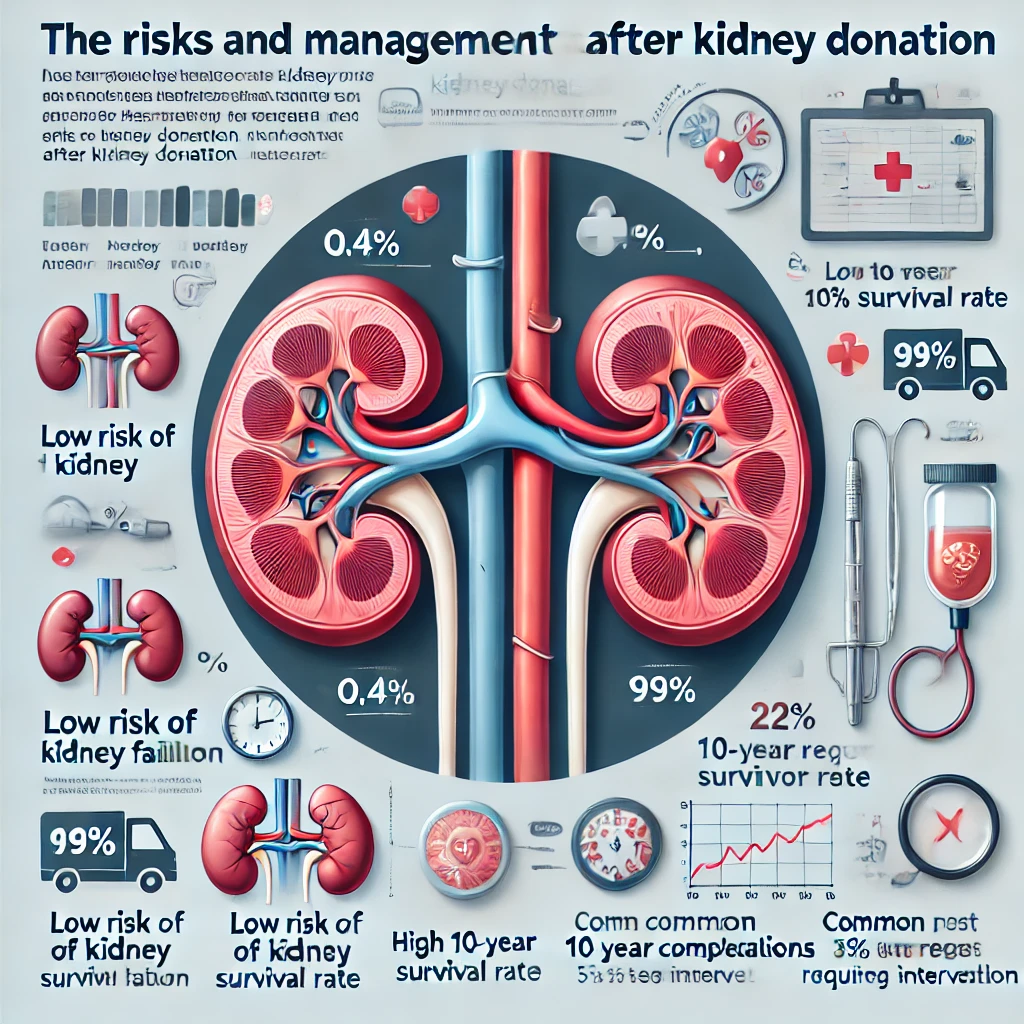
Risks of Kidney Function Decline After Kidney Donation and Post-Donation Management Guide
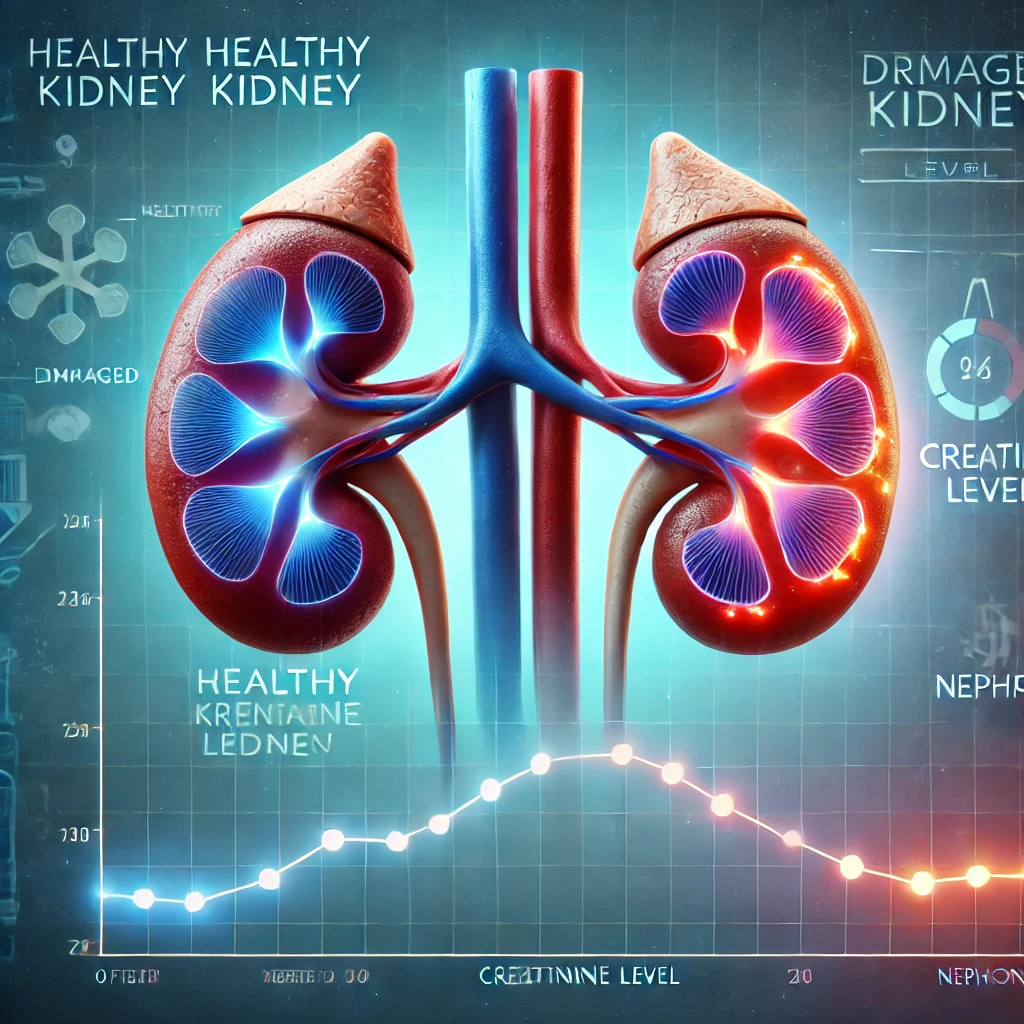
Living kidney donation is one of the most effective treatments for patients with chronic kidney disease. A recent study in New Zealand has confirmed that the long-term risk of kidney failure, cardiovascular disease, and complications… Risks of Kidney Function Decline After Kidney Donation and Post-Donation Management Guide