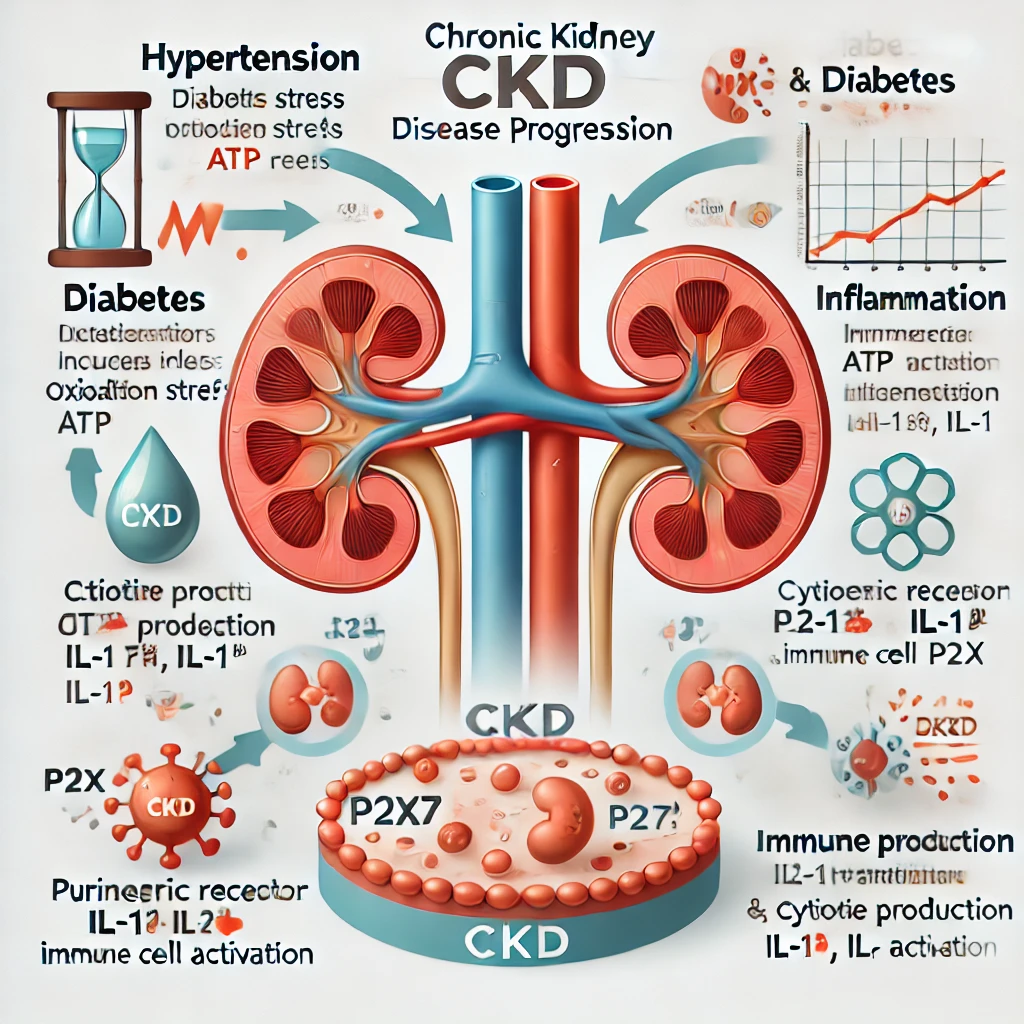
A New Therapeutic Mechanism for Chronic Kidney Disease (CKD) Discovered: The Role of Purinergic Receptor P2X7
1. What is the P2X7 Receptor? The Purinergic receptor P2X7 (P2X7) is an ionotropic purinergic receptor activated by adenosine triphosphate (ATP). It regulates the influx of calcium (Ca²⁺) and sodium (Na⁺) and the efflux of… A New Therapeutic Mechanism for Chronic Kidney Disease (CKD) Discovered: The Role of Purinergic Receptor P2X7