Perspectives on Awareness, Detection, and Treatment of Chronic Kidney Disease (CKD)
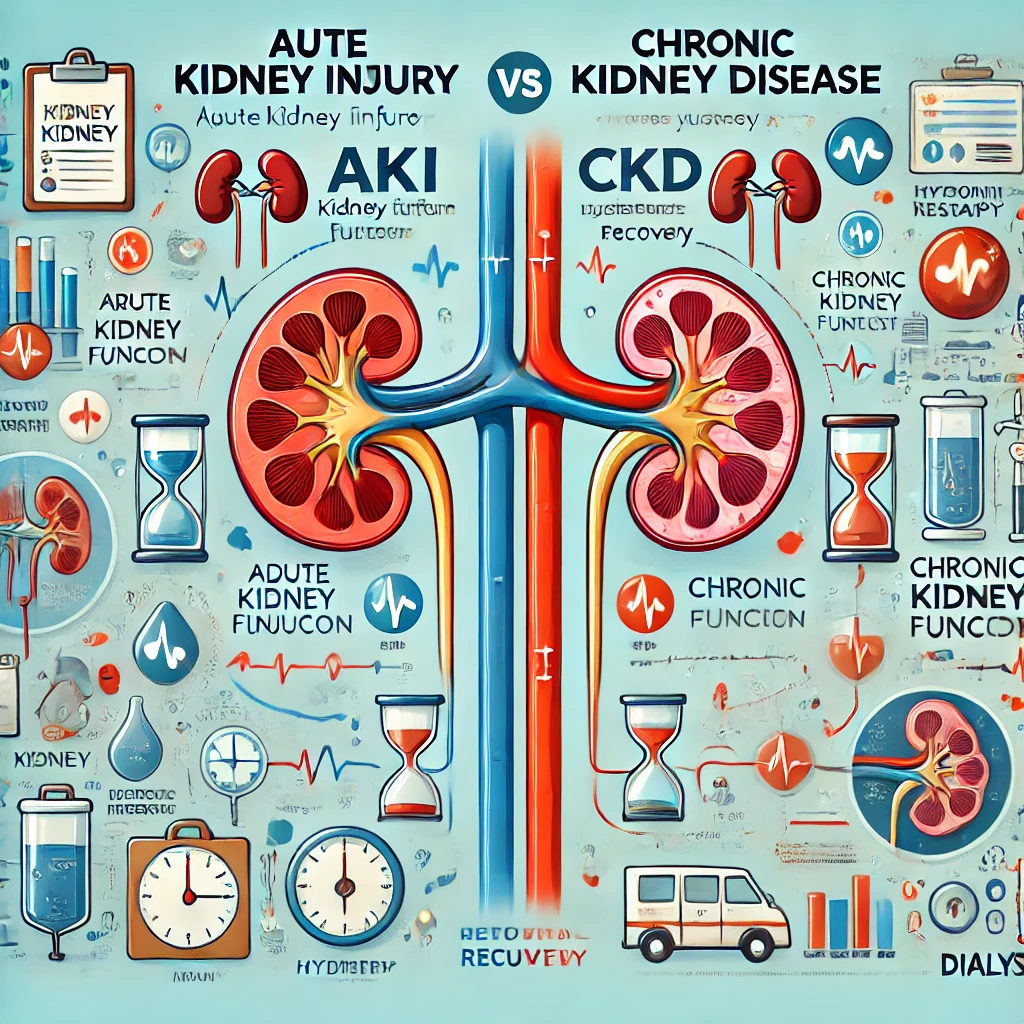
Chronic Kidney Disease (CKD) High-Risk Groups: Who Should Get Screened Early? Diabetes patients Hypertension patients Cardiovascular disease (CVD) patients Individuals with a family history of kidney disease Individuals with a history of acute kidney injury… Perspectives on Awareness, Detection, and Treatment of Chronic Kidney Disease (CKD)