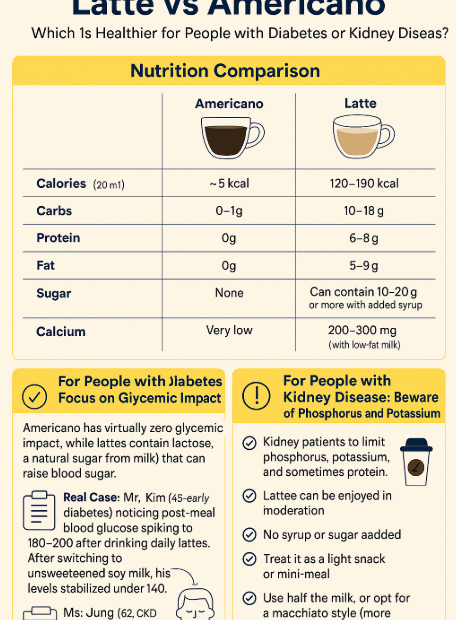
Latte vs Americano: Which Is Healthier for People with Diabetes or Kidney Disease?
Coffee is part of daily life — but how does your choice affect your health? Coffee is a staple in many people’s mornings, especially lattes and Americanos, which are among the most popular options. But… Latte vs Americano: Which Is Healthier for People with Diabetes or Kidney Disease?