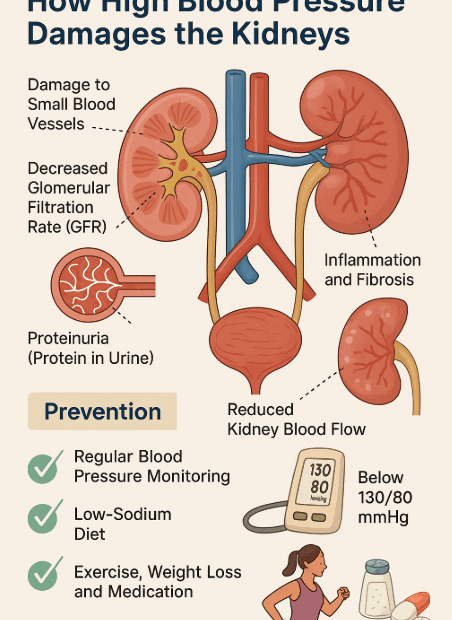
Hypertension: The Silent Killer That Destroys Your Kidneys
Introduction Hypertension is often called the “silent killer.” Without obvious symptoms, it gradually damages major organs in your body — and one of the most vulnerable targets is the kidney. The kidneys filter your blood… Hypertension: The Silent Killer That Destroys Your Kidneys