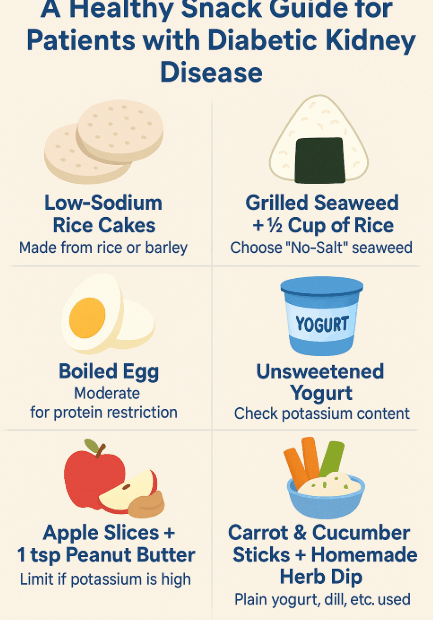
A Healthy Snack Guide for Patients with Diabetic Kidney Disease
Why Are Snacks Important for Diabetic Kidney Disease? Many people with chronic illnesses believe they should completely cut out snacks. For patients with diabetic kidney disease (DKD), who need to manage both blood sugar and… A Healthy Snack Guide for Patients with Diabetic Kidney Disease