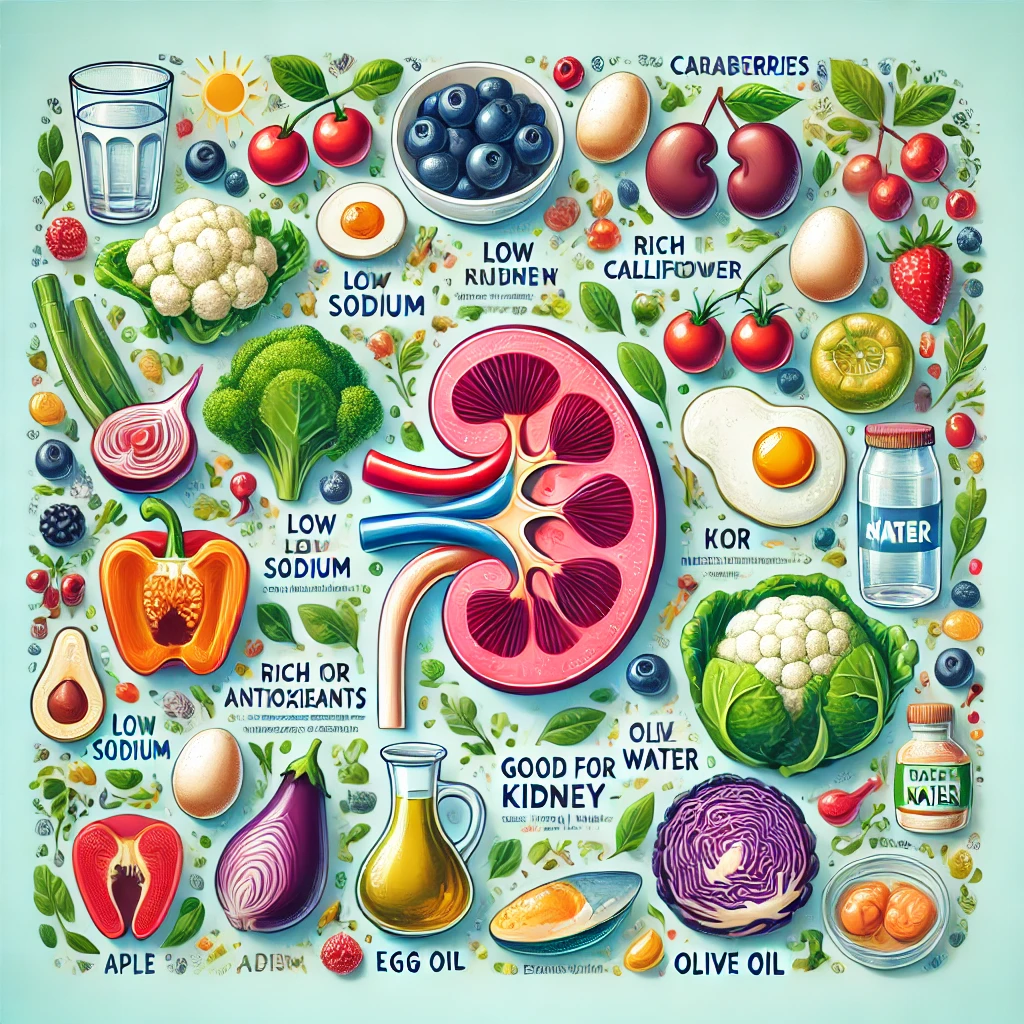
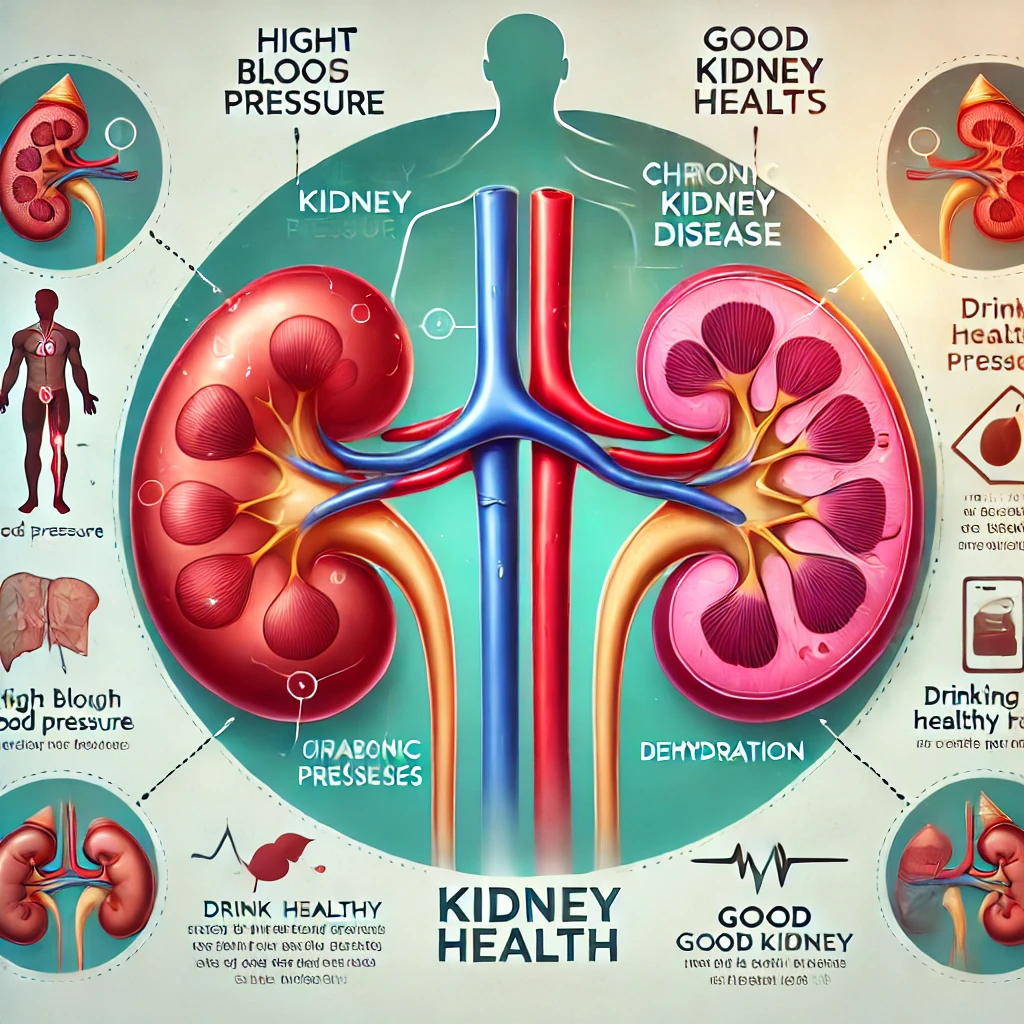
The Best Foods for Kidney Health, and Diet Guide
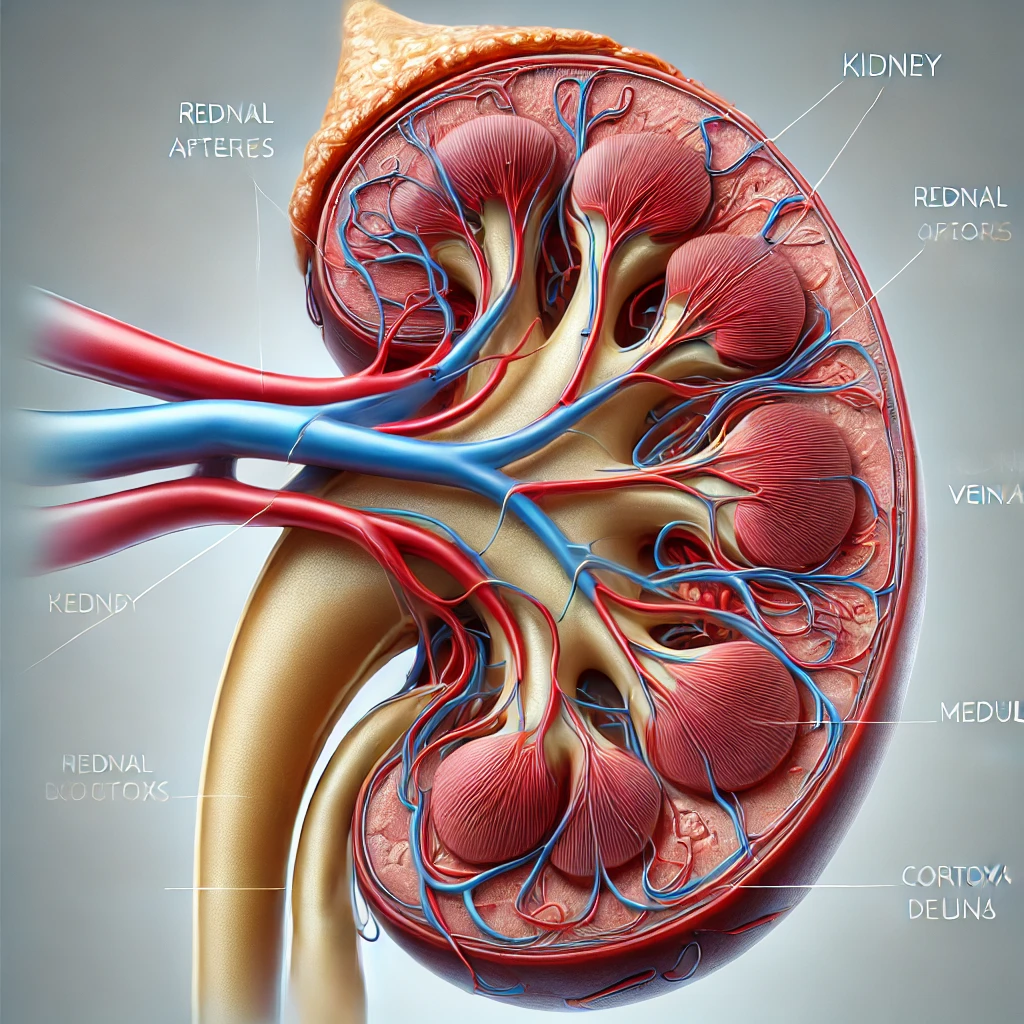
1. Proper Eating Habits for Kidney Health Foods for Kidney Health, The kidneys play a crucial role in filtering waste and regulating fluid balance in the body. However, poor eating habits and an unhealthy lifestyle… The Best Foods for Kidney Health, and Diet Guide