Should Chronic Kidney Disease (CKD) Patients Take Folic Acid?
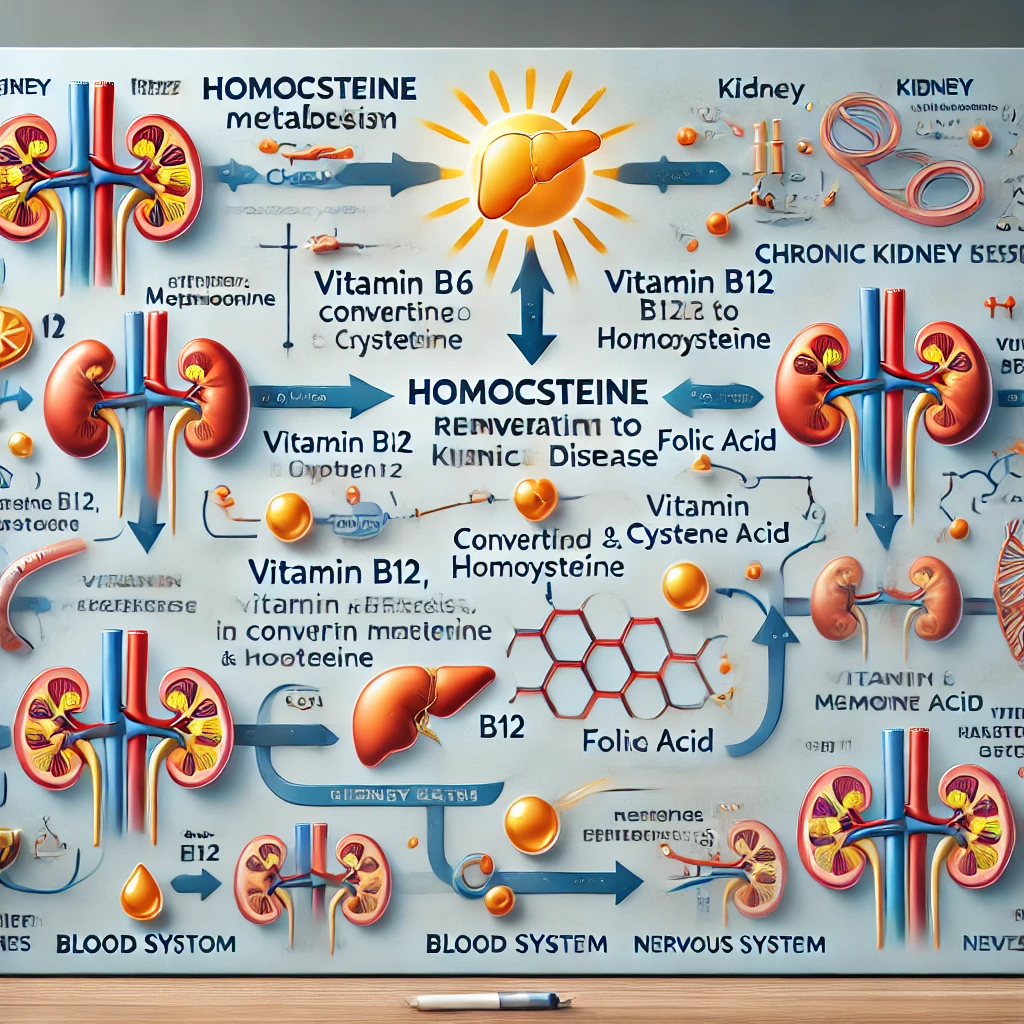
Many people wonder whether folic acid supplementation is necessary for patients with chronic kidney disease (CKD). To understand this, we need to first look at homocysteine. Homocysteine is an intermediate metabolic product formed during the… Should Chronic Kidney Disease (CKD) Patients Take Folic Acid?