Wegovy Alcohol Addiction: Research Findings and Potential Effects
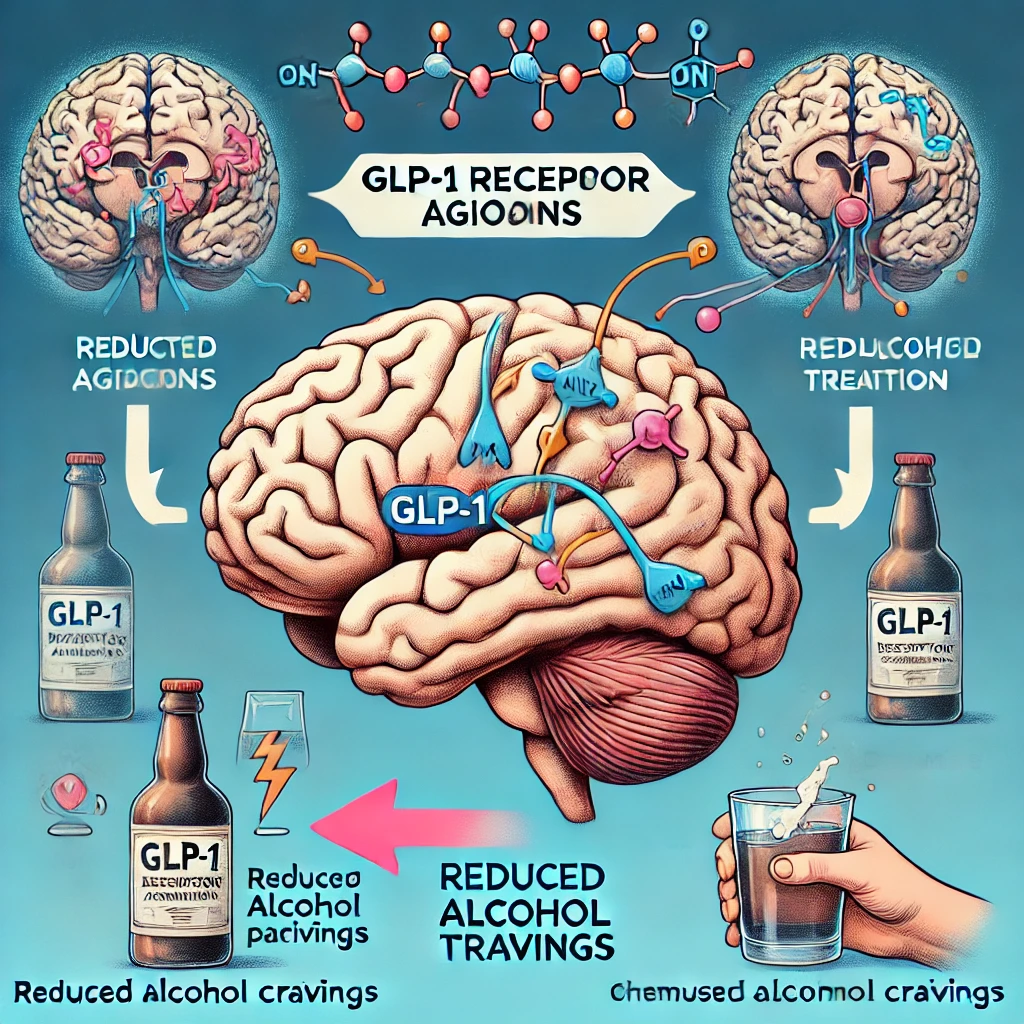
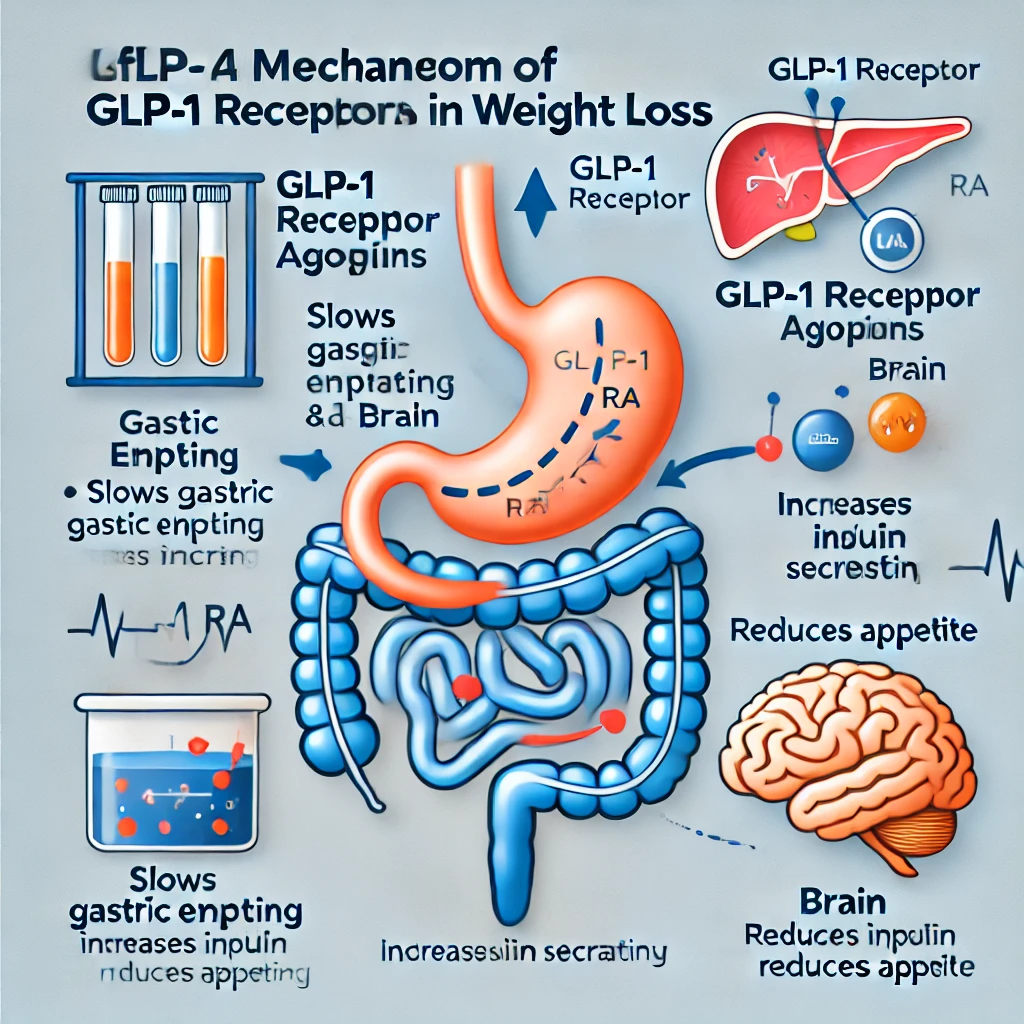
1. What Is Wegovy? Understanding GLP-1 Receptor Agonists Wegovy alcohol addiction, Wegovy (Semaglutide) is an injectable medication designed for weight loss. It contains Semaglutide, originally developed as a treatment for type 2 diabetes under the… Wegovy Alcohol Addiction: Research Findings and Potential Effects