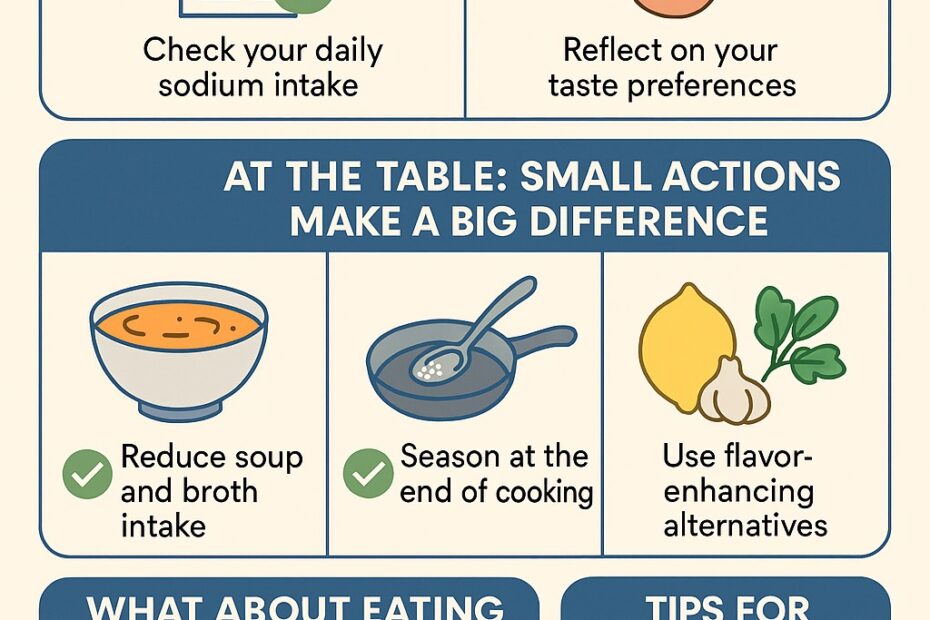
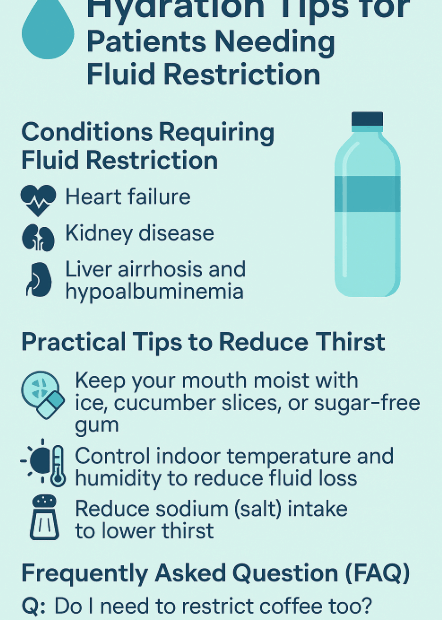
How to Start the Habit of Eating Less Salt
Introduction: Why Change the Habit of Eating Salty Food? Korean cuisine traditionally relies heavily on fermented sauces like soy sauce, doenjang (soybean paste), and gochujang (red chili paste), as well as salty side dishes like… How to Start the Habit of Eating Less Salt