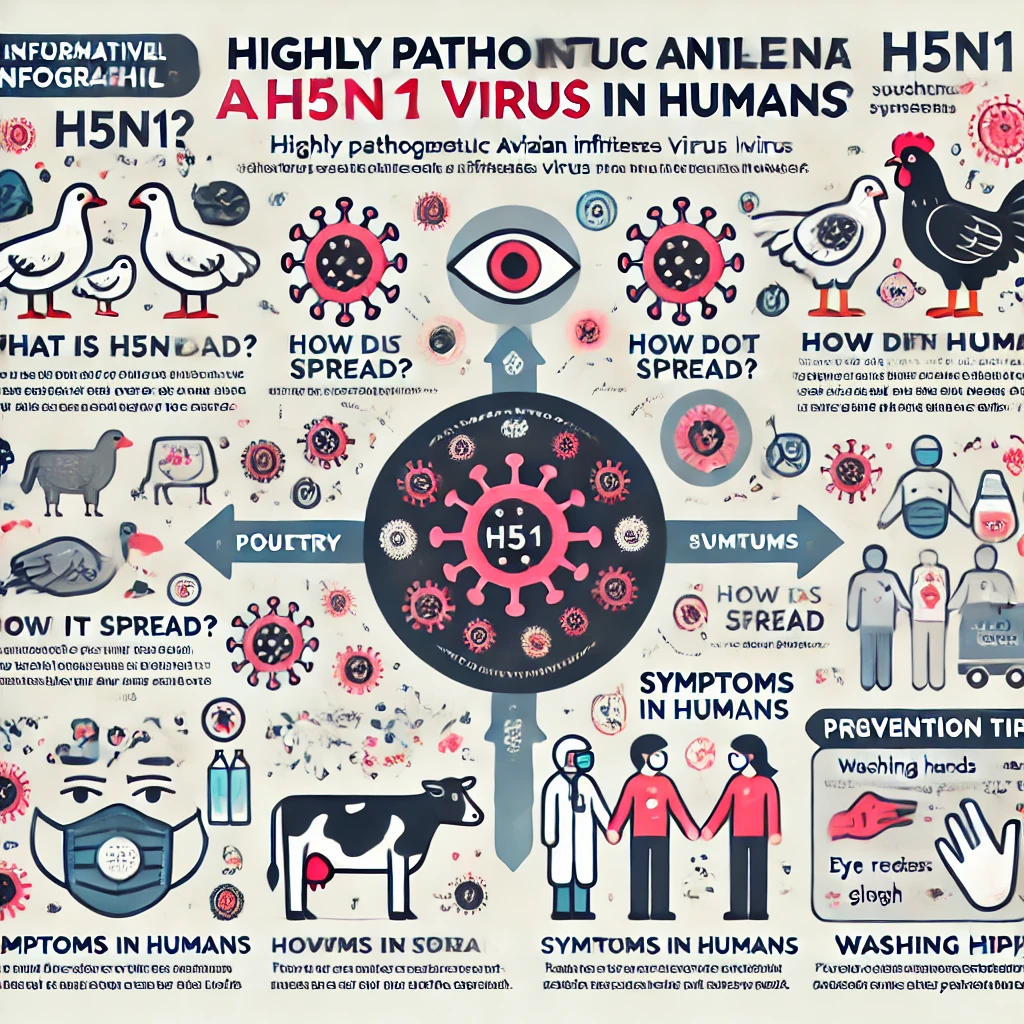
Highly Pathogenic Avian Influenza A(H5N1): Recent Human Infection Cases and Prevention Strategies
Summary Recently, cases of Highly Pathogenic Avian Influenza A(H5N1) virus transmission from dairy cows and poultry to humans have been reported in the United States. Between March and October 2024, 46 human infections were identified,… Highly Pathogenic Avian Influenza A(H5N1): Recent Human Infection Cases and Prevention Strategies