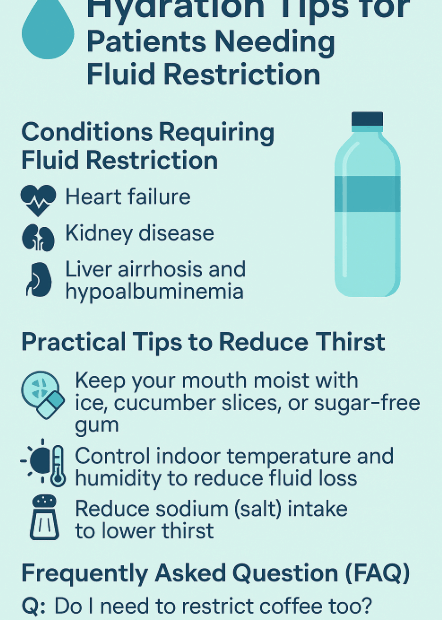
Managing Your Fluid Intake: A Complete Guide to Staying Healthy Without Constant Thirst (Especially for Chronic Kidney Disease and Heart Failure Patients)
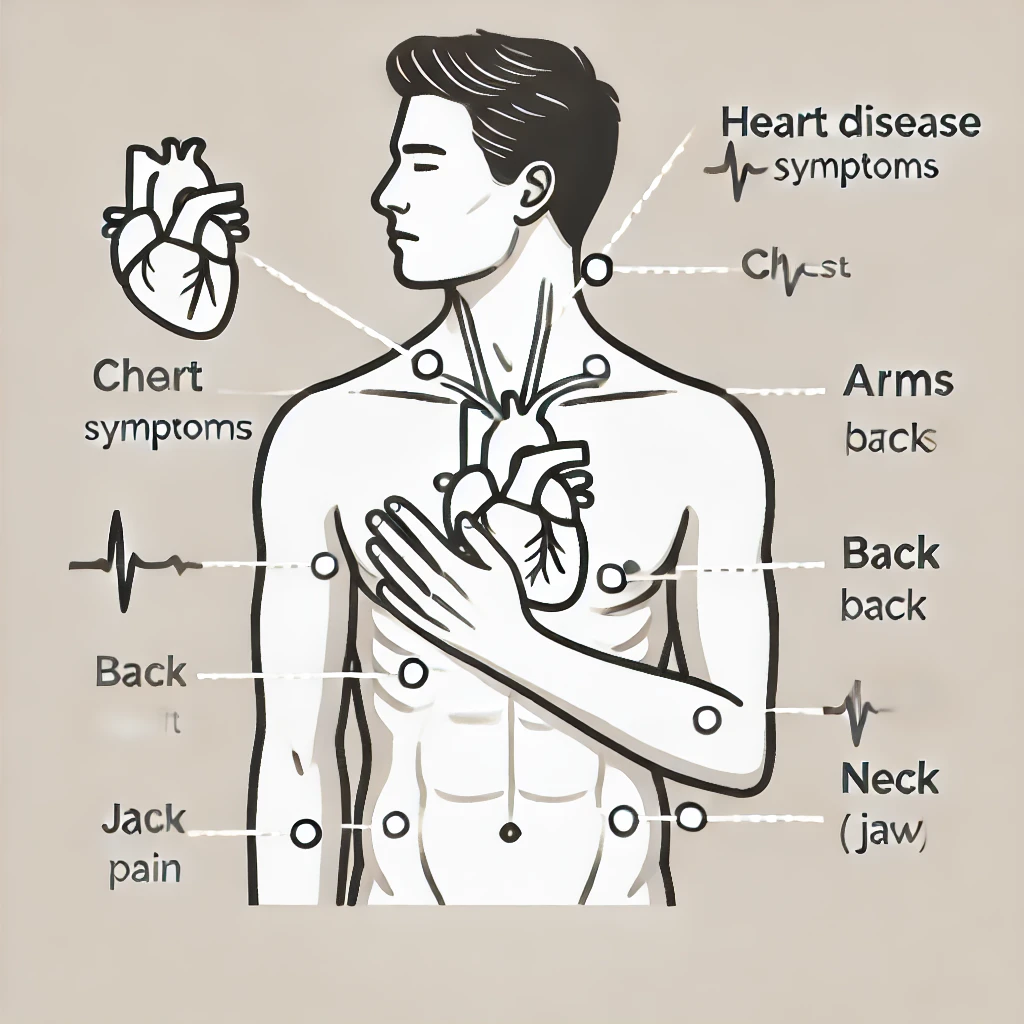
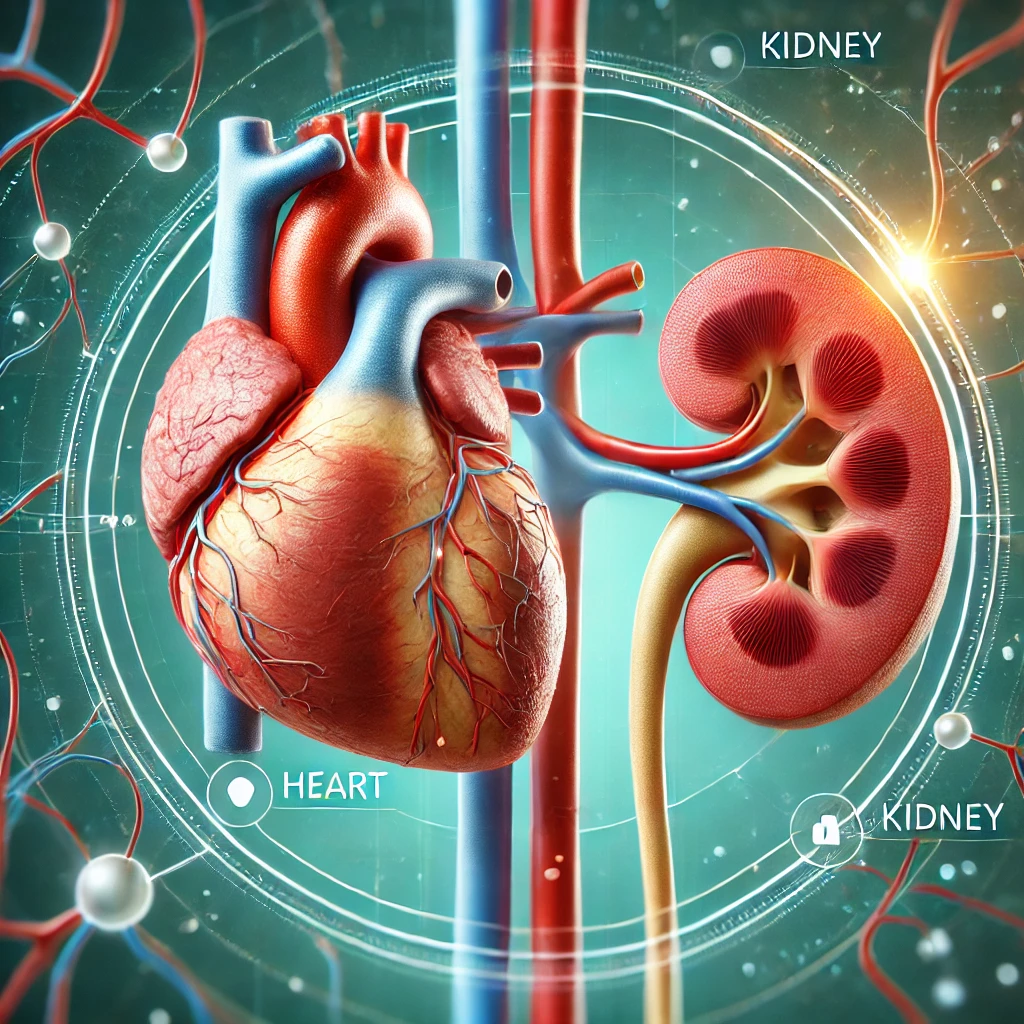
Water is essential for life, but for individuals with certain medical conditions, “drinking plenty” isn’t always the best advice. Patients with conditions like heart failure, chronic kidney disease (CKD), and those undergoing dialysis often need… Managing Your Fluid Intake: A Complete Guide to Staying Healthy Without Constant Thirst (Especially for Chronic Kidney Disease and Heart Failure Patients)