How Can Kidney Disease Patients Exercise Safely in the Summer?
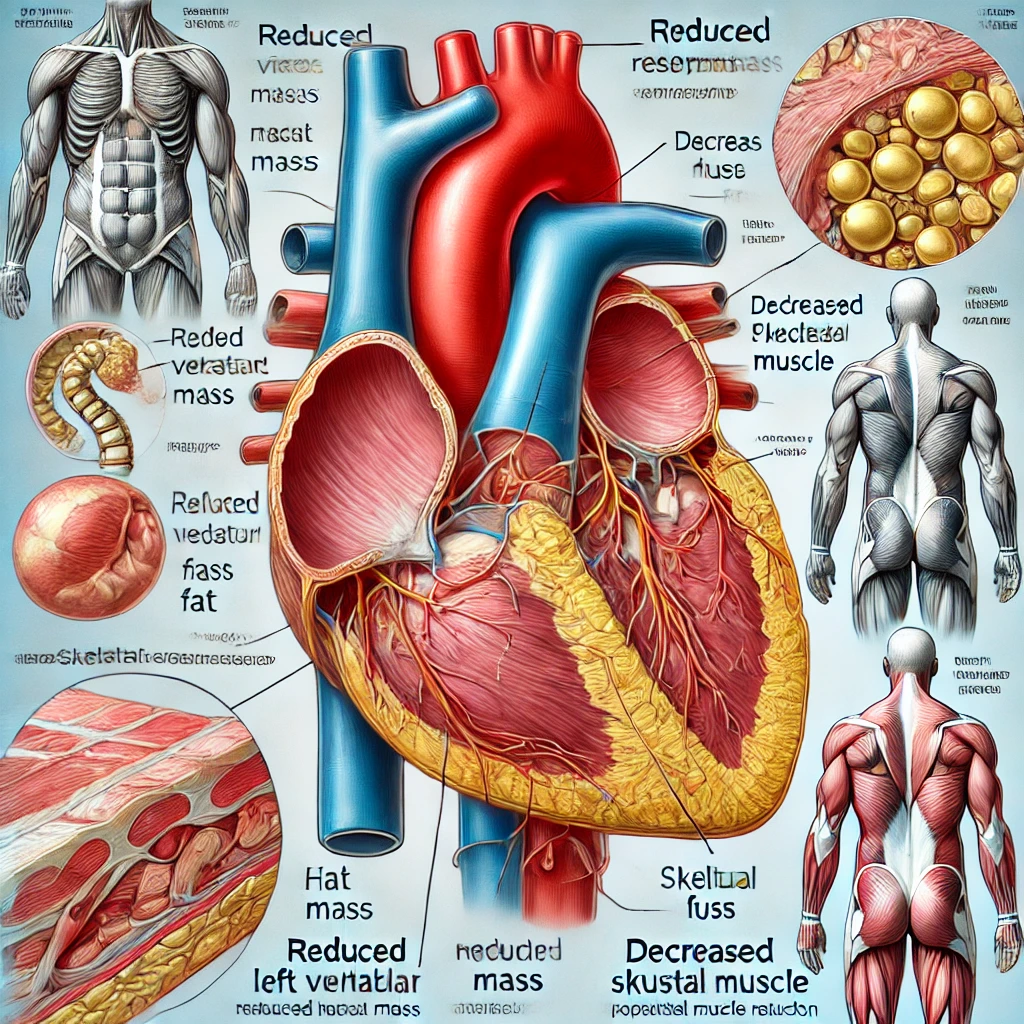
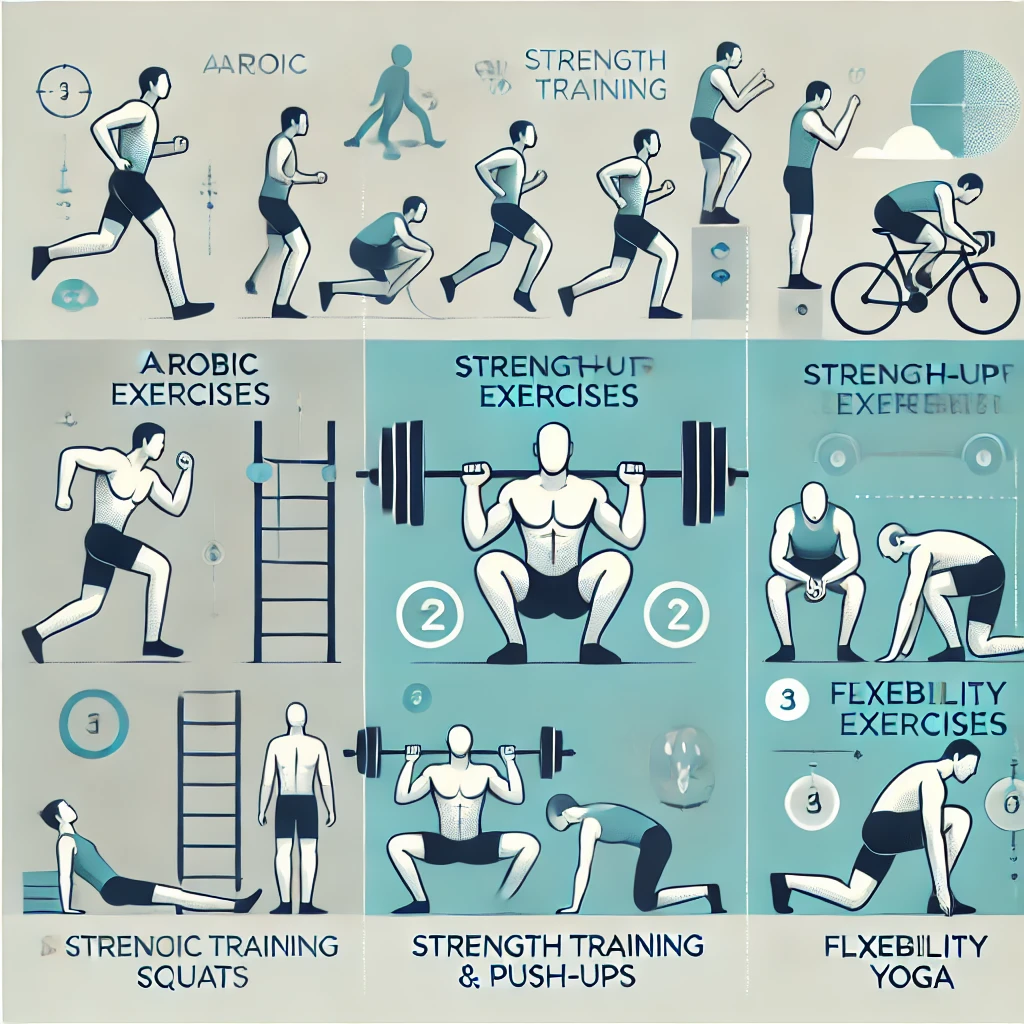
Summer’s high temperatures and humidity significantly increase the risk of dehydration and heat-related illnesses during exercise. Especially for patients with chronic kidney disease (CKD), impaired fluid and electrolyte regulation means extra caution is required. This… How Can Kidney Disease Patients Exercise Safely in the Summer?