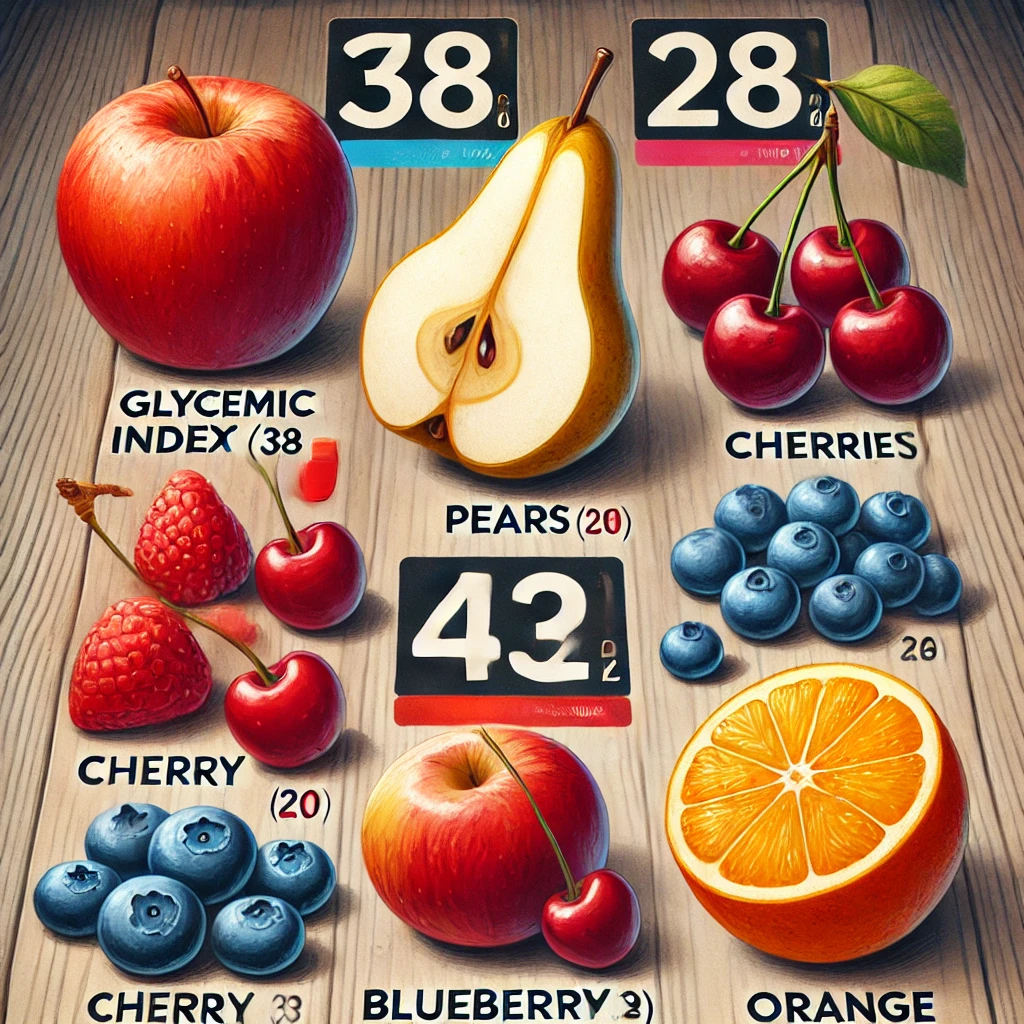
Be Cautious with Fruits! A Guide to Fruits for Diabetes Patients
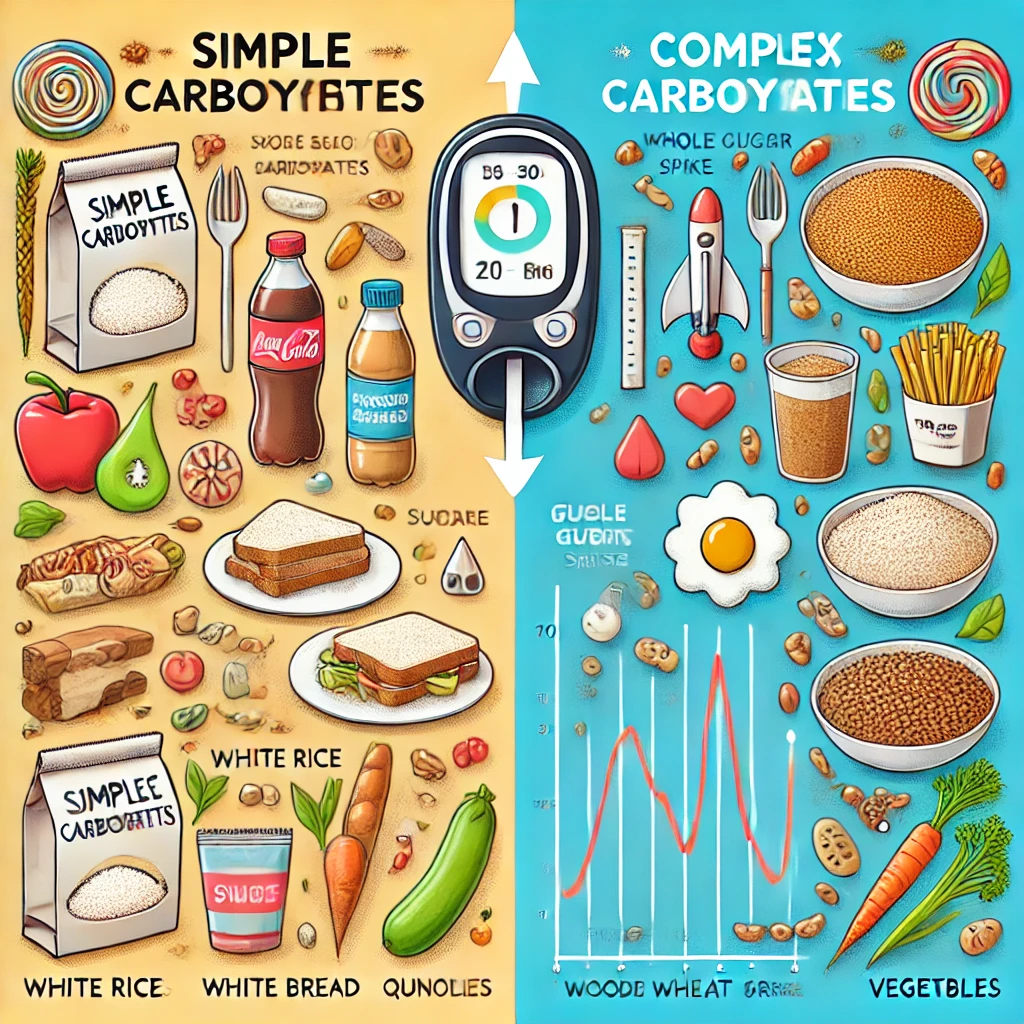
Fruits are rich in vitamins, minerals, and dietary fiber, making them an essential part of a healthy diet. However, diabetes patients need to carefully choose the right fruits to manage their blood sugar levels and… Be Cautious with Fruits! A Guide to Fruits for Diabetes Patients